by C. Vergara (LABS, DCMIC and Adjunct Prof. at MOX, Politecnico di Milano) and M. Domanin (Unità Operativa di Chirurgia Vascolare, Policlinico di Milano)
Carotid bifurcation is a preferential site for the development of atherosclerotic plaque. A major role in this process is given by the blood fluid-dynamics. In particular, low and oscillating wall shear stresses (WSS), i.e. large values of OSI, promote the plaque formation and restenosis.
Carotid endarterectomy (CEA, see Figure 1, top, left) is the most commonly performed surgical treatment to restore the patency of extracranial district. Closure technique after CEA still remains a debated major issue. Patch graft (PG) can be incorporated and the question arises as to whether it is better to employ PG or primary closure (PC). The standard use of PG has been endorsed by the guidelines of the most relevant scientific society of vascular surgery.
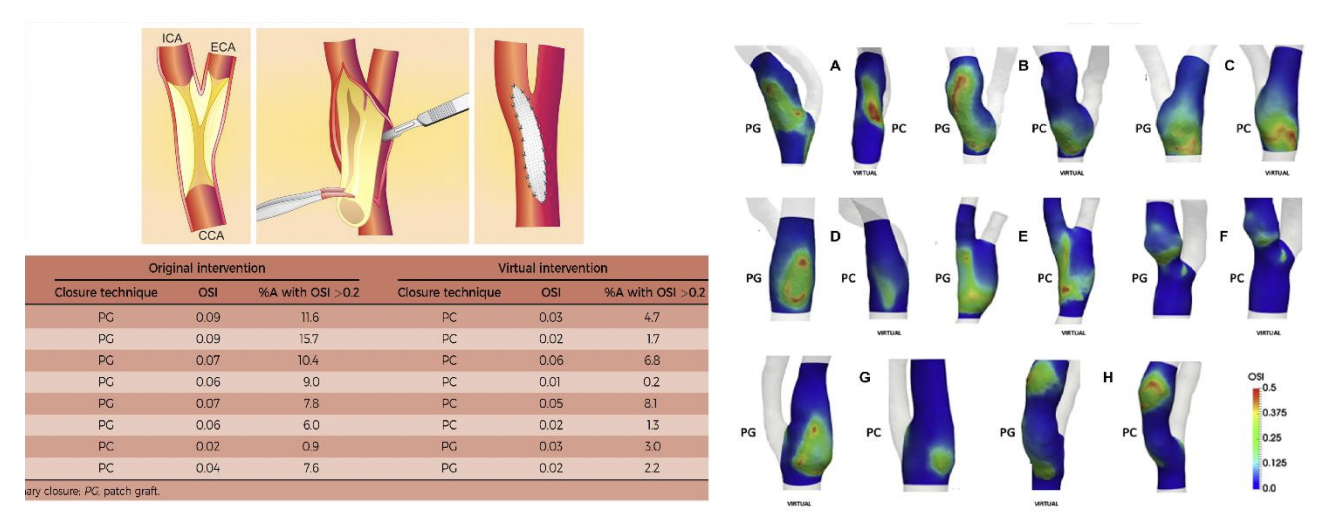
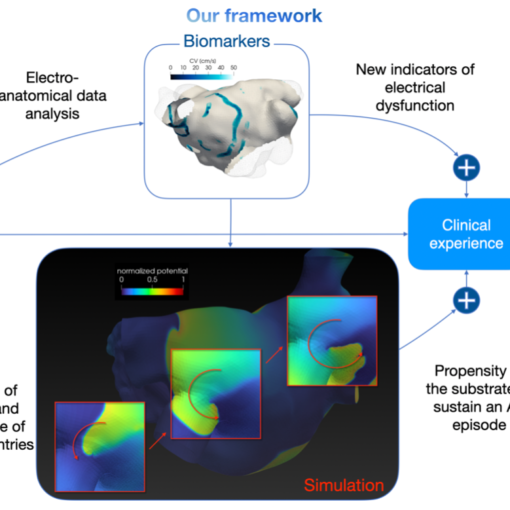
A success story. We provided a comparative CFD analysis between the two closure techniques performed in real geometries, where we have virtually designed PC in patients where PG was originally inserted, and viceversa. This allowed us to compare some WSS-based indices and to assess the effect of the closure technique on hemodynamics (see Figure 1, right).
Main clinical outcome. Our analysis supports the benefits of the selective use of PG, avoiding its use when CEA is performed only at the CCA or bulb level, or when ICA diameter is greater than 5.0 mm (see Figure 1, bottom, left).
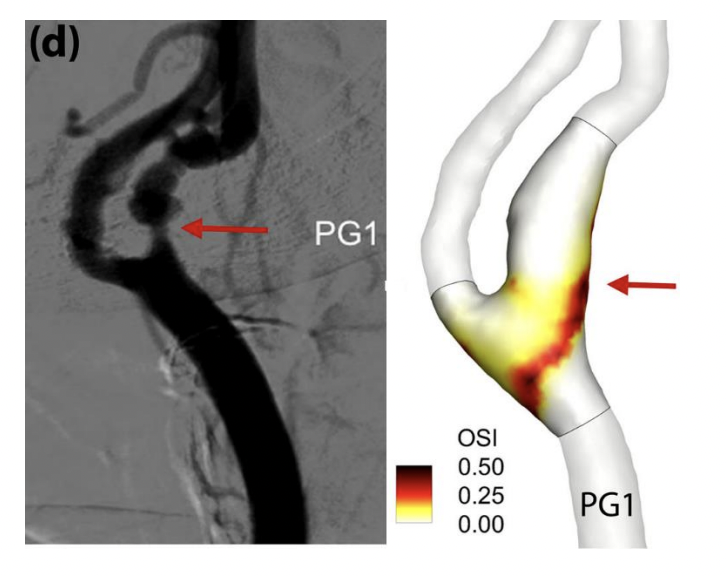
Towards clinical validation. One of the analyzed patients, who underwent to PG closure, after some years developed carotid restenosis, exactly in the region where we predicted that OSI was elevated (see Figure 2)
Clinical comment by M. Domanin, MD. “According to the CFD results, in my personal surgical praxis I have started to select the cases in which to insert PG after CEA. Nowadays, I’m limiting the use PG only in case of narrow ICA (< 5 mm), distal lesions or technical defects after CEA. In larger carotids, or lesions limited to the bulb region I prefer PC, that allows to reduce the time of cerebral ischemia during cross clamping, to simplify the overall surgical procedure, and reduce late complications such as PG infections or pseudoaneurysms. Moreover, this experience has stimulated a debate in the vascular surgical community, that is currently limiting PG closure going against current guidelines.”